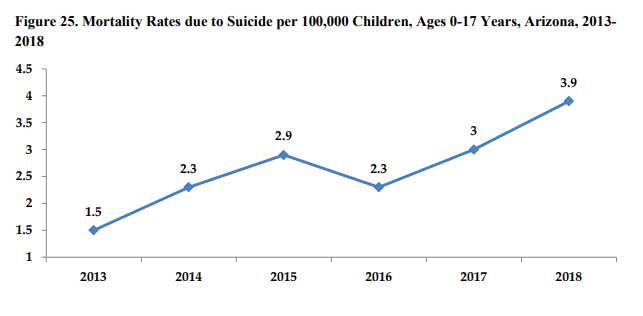
Suicide is clearly an important health issue in Arizona, especially for our youth. In 2020, there have already been new bills introduced to the Arizona State legislature that address child suicide prevention and mental health care. “Jake’s Law,” introduced last week, aims to increase behavioral health services, create a suicide mortality review team, and enforce federal parity laws (Whaley, 2020). It is important that we are aware of the role ethics plays in health policy as we review these bills decide which ones to advocate for or against.
I remember taking my undergraduate nursing ethics class, reading the Code of Ethics for Nurses with Interpretive Statements (American Nurses Association [ANA], 2015), and making note-cards about all the principles of ethics in nursing. Back then, I focused on how these principles would affect my day-to-day bedside nursing practice. Now, as a doctoral nursing student, I have the opportunity to see how nurses are called to be involved in policy. As Provision 7.3 of our code of ethics states, nurses are responsible for contributing to policy development on all levels of healthcare (ANA, 2015). We have a duty to participate in the political arena by leading, mentoring, advocating, and even serving as representatives to ensure that healthcare policies are ethical, evidence-based, and effective (ANA, 2015).
Thankfully, we live under a government where the people can create policy and get policy enacted. Therefore, the ethics of a public policy and the policymaking process is related to the ethics of the people making the policy decisions (Longest, 2010). Policy makers must consider the ethical impact of a new policy with regards to the four ethical principles that guide policy making: autonomy, justice, beneficence, and nonmaleficence (Longest, 2010). (These are all ethical principles of nursing, too!) They must understand how it will affect autonomy, the concept that relates to an individual’s right to make their own decisions. In order to adhere to this principle, the policymaking process must be truthful and honor privacy (Longest, 2010). Policy must be sure to adhere to the principle of justice; the principle related the fairness (Longest, 2010). Fairness can be subjective, so there are different ethical perspectives that can guide this. Additionally, policymaking is to uphold beneficence. Beneficence is the principle that relates to doing good and providing the least amount of burden (Longest, 2010). Lastly, Longest (2010) describes nonmaleficence as the principle “to do no harm” (p. 208). Policymakers must be cognizant of the possibility that some policies may have negative effects.
With these principles in mind, one can begin to discuss how ethical principles relate to policymaking to help with suicide prevention. We know that policy must respect the rights of the people, be fair, and do the most good while doing no harm.
There has been significant debate over the ethics related to suicide. One may argue that it is a person’s right to decide to take their own life. But, when a person is in crisis their decision-making capacity is impaired, and therefore it is not just to allow someone to take their own life, especially because evidence shows that the majority of people who complete suicide have a mental illness (Kelly & Dale, 2011). Many suicide prevention measures impede on one’s rights in order to ensure that they have the opportunity to receive treatment. When a person reports having thoughts to harm themselves, confidentiality can be breached, their belongings can be taken away (i.e. weapons), and they can be forced to get treatments. These measures must be taken in order to give them the opportunity to obtain their decision-making capacity and to be non-suicidal again.
The Arizona Child Fatality Review Program (2019) team has decided that ALL child deaths by suicide are preventable. Therefore, there is a need for interventions to prevent child suicide. In addition to actual mental health services and treatment in community and hospital settings, there is a call to address the social determinants of health related to suicide (Fitzpatrick, 2018). There are numerous opportunities for policymakers to make a positive impact on suicide prevention in a way that adheres to the ethical principles discussed.
“Jake’s Law” (SB1523 and HB2764) introduced to Arizona’s legislature by Sen. Kate Brophy McGee and Rep. Jeff Weninger, includes these provisions:
- “Requires insurance cards issued in Arizona to clearly identify which governmental agency to contact for questions or to file complaints.
- Requires the Department of Insurance to establish a consumer-friendly webpage containing resources pertaining to mental health parity, a step-by-step guide on how to file parity violation complaints, and a summary regarding insurers’ compliance with mental health parity laws.
- Prohibits an insurer from denying a claim for mental health or substance abuse benefits based solely on the grounds that the service was provided in an educational setting or was court ordered.
- Establishes a Mental Health Parity Advisory Committee to provide the Director of the Department of Insurance advice on case management, discharge planning, and expedited review and appeals processes for cases involving suicidal ideation.
- Expands access to behavioral health services in schools be establishing an $8 million fund to help students covered by private insurance but who are unable to afford their copay or deductible.
- Establishes and appropriates $100,000 for a Suicide Mortality Review Team within the Department of Health Services. (Whaley, 2020)”
From an ethical stand point, these laws could increase individual’s autonomy by allowing them better access to the care that they need. The provisions adhere to the principle of justice by making the insurance companies comply with existing federal parity laws. And they can do good for the people of Arizona by providing more treatment and resources to youth with mental health issues. However, it may cause a burden by increasing premiums for insurance payers and taxpayers. What other ethical implications of these provisions do you see?
It will be interesting to see how these bills progress and I look forward to discussing other new bills that have been introduced to the Arizona State legislature this year in future blogs.
References
American Nurses Association (2015). Code of ethics for nurses with interpretive statements. Silver Spring, MD: Nursesbooks.org Retrieved from https://www.nursingworld.org/coe-view-only
Arizona Child Fatality Review Program (2019). Arizona child fatality review program: Twenty-sixth annual report. Retrieved from https://www.azdhs.gov/documents/prevention/womens-childrens-health/reports-fact-sheets/child-fatality-review-annual-reports/cfr-annual-report-2019.pdf
Fitzpatrick, S. J. (2018). Reshaping the ethics of suicide prevention: Responsibility, inequality, and action of the social determinants of suicide. Public Health Ethics, 11(2), 179-190. https://doi-org.ezproxy1.lib.asu.edu/10.1093/phe/phx022
Kelly, C., & Dale, E. (2011). Ethical perspectives on suicide and suicide prevention. Advances in Psychiatric Treatment, 17(3), 214-219. doi: 10.1192/apt.bp.109.007021
Longest, B.B. Jr. (2010). Health policymaking in the United States (5th ed.). Chicago, IL: Health Administration Press.
Whaley, M. (2020). New Arizona measure tackles suicide, mental health. Retrieved from https://stateofreform.com/featured/2020/02/new-arizona-measure-tackles-suicide-mental-health/